By Randy Mulyanto and Beh Lih Yi
JAKARTA/KUALA LUMPUR, Jan 27 (Openly) - First it was the neighbours who started avoiding Indonesian food hawker Titi Amaliyah. Then regular customers stopped buying her traditional noodle snacks when word spread that she had been diagnosed with leprosy.
Since her diagnosis last year, Amaliyah and her family have been dependent on her husband's income from odd jobs, which has dwindled due to the coronavirus pandemic. With three children, they are struggling to put food on the table.
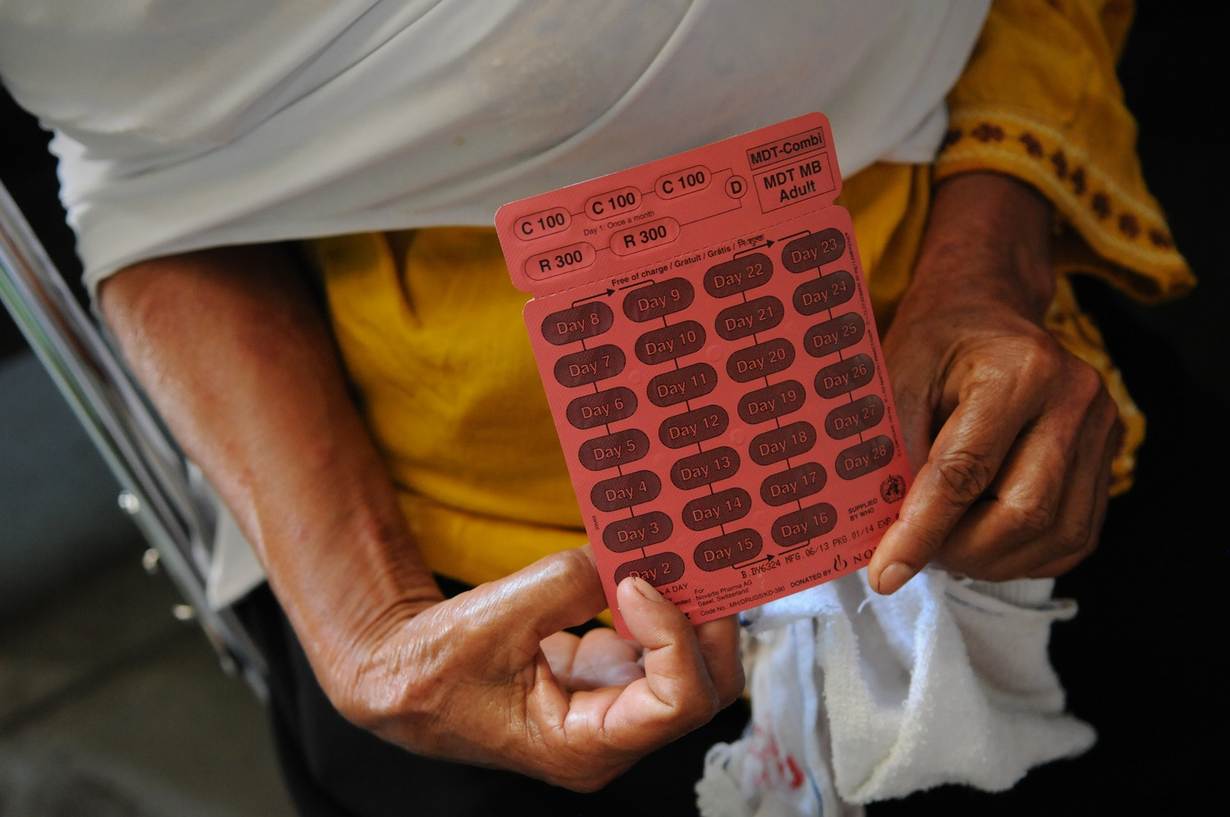
"It's a mental burden for me and it affects my family's income," said Amaliyah, 44, who is being treated for the age-old disease that can be cured with a combination of drugs.
"I just want the red spots on my skin to disappear," she told the Thomson Reuters Foundation by phone from Indonesia's central Java island, looking to the days when she can be accepted by her close-knit community again.
Amaliyah is one of thousands of Indonesians living with leprosy, a disease caused by bacteria spread through droplets from the nose and mouth that causes nerve damage and lesions on the skin.
It often carries a stigma that pushes sufferers to live on the margins of society, while fears of economic and social exclusion mean many do not get tested or treated.
Indonesia reported more than 17,000 new cases in 2019, the third highest in the world after India and Brazil, according to the World Health Organization (WHO).
And as affected countries focus on combatting COVID-19, health experts fear leprosy is being pushed further to the margins.
TIME BOMB
Leprosy is one of the oldest known diseases, affecting the poorest and most marginalised communities.
Millions have been cured since 1981 with a multidrug therapy and the number of cases worldwide has plummeted from a total of 10-12 million in the mid-1980s to about 200,000 new cases each year now.
But it still exists in more than 100 countries, and millions live with its effects.
Leprosy is one of the neglected tropical diseases (NTDs) that affect more than 1.7 billion people in some of the world's poorest countries.
These diseases disable and disfigure sufferers, often leaving them isolated and unable to earn a living, but they can be treated.
On Saturday, the WHO will mark World NTD Day after launching a roadmap setting out global targets to tackle 20 of the diseases including leprosy by 2030.
The roadmap comes amid concerns that the pandemic is hampering efforts to tackle NTDs like leprosy, which health advocates say could be a ticking health time bomb for Indonesia, a country of 270 million where access to healthcare was challenging even before.
"We believe there will be a large-scale transmission in the coming two to five years," said Indonesian leprosy survivor Paulus Manek, who heads Permata, a charity helping sufferers.
Manek said local health facilities were overwhelmed, causing delays in accessing medicines, and COVID-19 movement restrictions had prevented his charity from operating. Indonesia has more than a million coronavirus cases.
"We're not going all out to prevent leprosy, the contacts are not traced. Even though the government has good regulations in place, enforcement on the ground is patchy," said Manek, 40.
Indonesia's health ministry did not reply to a request for comment. The ministry said last year it was working to raise public awareness about leprosy and in September it launched online training for health workers to detect new cases.
NLR Indonesia, a non-profit organisation that works with Indonesia to eliminate leprosy, said officials had introduced solutions including prescribing medications for a longer period than the usual one month.
But it said detection of new cases in 34 districts it works in had fallen 40% in the first six months of last year compared to 2019, suggesting resources to trace and spot new patients had been shifted elsewhere.
"These are not just worries. If we compare the data... this shows the efforts have gone down last year although this is inevitable due to COVID-19," said Asken Sinaga, NLR Indonesia's executive director.
"We hope the government can keep its attention on leprosy despite its current priority on COVID-19.
"The awareness on leprosy is low in Indonesia and there is widespread stigma. Some doctors are not aware leprosy is still an issue in Indonesia and they don't know how to diagnose it," Sinaga added.

STIGMA AND MYTH
Yet Thoko Elphick-Pooley, director of the Uniting to Combat NTDs coalition, argues the global mobilisation against COVID-19 can provide the push needed to tackle diseases that have long been neglected.
"We can use the impetus we have now from COVID to deal with some of those diseases, like leprosy, which was around thousands of years ago and is still around," she said.
"We get outraged by diseases that kill, but not by diseases that disable."
The WHO declared leprosy was no longer a public health problem in 2000, when the number of cases fell to less than one in 10,000 people.
Transmission is believed to take place during the long incubation period, between three and five years on average, before the disease can be diagnosed. Leprosy symptoms can take up to 20 years to appear.
One way of stopping the disease from spreading is to trace all contacts of patients and give them preventative treatment.
But stigma and myths associated with leprosy that go back centuries can deter people from seeking treatment, leading to permanent disability.
"Late diagnosis leads to late treatment and more risk of developing disabilities," said Liesbeth Mieras, head of the medical technical department at Netherlands-based non-profit NLR, which works in five countries to eliminate leprosy.
"The COVID-19 pandemic has diverted health staff to work solely on COVID-19 related activities, which has led to a substantial reduction in the number of new patients detected."
Many affected by leprosy still bear the scars even after they are cured.
"For COVID, it is a disease inside your body, people cannot see it," said Dasuki Hidayat, 40, who was cured from leprosy in 2000 but suffered permanent nerve damage to his hands.
"With leprosy, when people hear the name, they are still disgusted. The stigma towards leprosy is still very high."
This story is one in a series supported by Uniting to Combat Neglected Tropical Diseases
RELATED STORIES
Leprosy still affects millions but can be wiped out - expert
No medicine, no food: Coronavirus restrictions amplify health risks to LGBT+ people with HIV
Africa's miners face new TB threat as pandemic disrupts treatment
(Reporting and writing by Beh Lih Yi @behlihyi in Kuala Lumpur, Randy Mulyanto in Jakarta; Editing by Claire Cozens. Please credit the Thomson Reuters Foundation, the charitable arm of Thomson Reuters, that covers the lives of people around the world who struggle to live freely or fairly. Visit http://news.trust.org)
Openly is an initiative of the Thomson Reuters Foundation dedicated to impartial coverage of LGBT+ issues from around the world.
Our Standards: The Thomson Reuters Trust Principles.